Here's the good news from the Philippine Daily Inquirer--
Jobs in UK still await RP health workers
By Jerome Aning
Philippine Daily Inquirer
First Posted 20:19:00 12/28/2008
MANILA, Philippines--Filipino nurses and other health care professionals seeking overseas employment need not worry about losing job opportunities in the United Kingdom, as there are many vacancies there that have to be filled up in the next few years.
A recruitment industry expert made this assessment on Sunday as he identified the British health care sector as one that has been in need of health care professionals, regardless of the financial slump affecting many European countries.
"The health care industry in UK is mainly funded by taxpayer's money and is managed by the National Health Service (NHS) which is the largest employer in the UK," Emmanuel Geslani, a consultant of several Manila-based recruitment agencies, told reporters.
Geslani, however, said the NHS system has been "failing" in matters of primary care and hospital services due the lack of nurses and senior carers resulting in lack of hospital beds and personnel to attend to the sick.
He cited a recent study of current vacancies in nursing and senior carers that showing nearly 10,000 vacancies, resulting in the poor delivery of services in hospitals and care homes.
With the aging population of the UK calculated to reach 30 percent for the entire country by 2010 some 10 million senior citizens would need better services from care homes, the study said.
"Thousands of Filipino nurses can fill up the gap in the nursing shortage in the UK by entering the country as student nurses and at the same time expand their knowledge and experience in British schools," Geslani suggested.
The projected vacancies are so worrisome that some placement agencies in Britain have been recruiting nursing students even before they graduate or take their licensure exams, according to Geslani.
He added that one British consultancy firm, realizing the need to "capture" much needed health care professionals, pioneered a "study-and-work" placement scheme for nursing students and the so-called "under-board graduates" to boost their academic qualifications and help them meet UK standards.
The International Student Advisors Inc. offers a plan whereby students and graduates of social, health care and international nursing degrees from the Philippines would be temporarily employed, with pay, in care homes and hospitals in the UK while completing their units or taking additional ones in accredited British universities.
"Through the scheme, the students can understand what actually happens in the place of work and undertake projects in preparation for their essays and exams. Under the vocational work placement of at least 30 hours a week, the students can cover their living costs and tuition fees," Geslani explained.
He said the Makati City-based ISA, which recently expanded its recruitment activities in eight provinces, already sent over 600 Filipino health care professionals to enroll in renowned UK schools such the Anglia Ruskin and Hertforshire universities for additional nursing degrees and in preparing for taking up the British overseas nursing program assessment
Monday, December 29, 2008
It's still OK in the UK for Philippine Health Workers
Posted by
albularyo
at
1:21 AM
0
comments
![]()
Labels: Careers
Wednesday, December 10, 2008
US relaxes visa requirements for nurses
Says shortage may become national security concern MANILA, Philippines -- The US government has issued a directive to relax visa procedures for foreign nurses after the Department of Homeland Security (DHS) acknowledged the acute shortage of the health care professionals there. The directive, Processing of "Schedule A" Nurse Visas, which can be accessed at http://www.hammondlawfirm.com/downloads/CIS_Ombudsman_Schedule_A.pdf, released on December 5, noted that "visa availability" remains the main obstacle for foreign nurses seeking work in the US, whether they intend to become immigrants or not. The Office of the Citizenship and Immigration Services (CIS) Ombudsman of the DHS, which released the directive, said that while the Department of Labor (DoL) has already allowed employers to bypass the first step in the hiring process, it enjoins the USCIS to adjust its procedures as well. "Specifically the USCIS should separate and prioritize, as well as centralize, its process for [Schedule A] applications in accordance with Congress' expressed concern over the national nursing shortage and to ensure consistent adjudication of applications," it said. The DoL has designated registered nurses (RNs) as a Schedule A occupation, meaning there are insufficient US nurses able, willing, qualified, and available to fill the vacancies. The designation also means the wages and working conditions of US nurses will not be adversely affected by the employment of foreign nurses. The CIS Ombudsman noted that all the criteria needed for automatically expediting such applications from employers apply to the US nursing shortage -- "extreme emergent situation," "humanitarian situation," and "compelling interest of the service." It noted that the shortage will impact on the quality of patient health care in the US. "The shortage of RNs and an increased workload for current nurses is a threat to the quality of patient care," it said. On the other hand, centralizing the applications would result in "more efficient processing times and improved consistency in the adjudications." Lawyer Ibaro Relamida, counsel of Sentosa Recruitment Agency, said the directive will take effect right away. He said Sentosa's 600 Filipino nurses are expected to get their EB3 visas within the month. "Last month, we were able to send only 20 nurses to the US," he told INQUIRER.net. "We still have the visas of 1,000 being processed." A 2007 study of the US Department of Health and Human Services shows that the US would need 1.2 million nurses by 2014, about half a million to meet the demand, and 700,000 more to replace those leaving the profession. In its report, the CIS Ombudsman cited a warning from the Americans for Nursing Shortage Relief to the House Subcommittee on the Nursing Crisis that the "shortage could result in serious national security and health concerns if there is a pandemic flu or other man-made or natural disaster, and the United States does not have adequate health care resources to respond." The CIS Ombudsman acknowledged that the US cannot expect to meet the growing demand for nurses. It also recognized that the piecemeal approach to visa applications for foreign nurses would not work. Currently, foreign nurses can work in the US if they have any of the following visas: * H1C non-immigrant visas, three-year visas for nurses in specified areas with nurse shortage, were issued to 49 in 2007 and 110 in 2008; * TN non-immigrant visas, also three-year visas with an option to extend in increments of three years open to Canadians and Mexicans, were issued to 194 in 2006 and 356 in 2007; * H1-B non-immigrant visas, for nurses in specialized occupations, were issued only to 38 in 2006, 66 in 2007, and 136 in 2008; * EB3 immigrant visas, which gives foreign nurses permanent legal residence (the so-called "green card"), are the ones on DoL's Schedule A. Although the most common visas issued for foreign nurses, they depend on visa availability as determined by the Department of State. In 2007, a total of 9,689 such visas were issued.
By Veronica Uy
INQUIRER.net
First Posted 14:49:00 12/11/2008
Posted by
albularyo
at
7:47 PM
1 comments
![]()
Labels: Careers
Friday, December 5, 2008
Pork & Brain
This is one of the reasons why I want my meat, well done… ;)
Words of the Day: Neurocystercercosis and Taenia Solium
Posted by
albularyo
at
8:13 PM
1 comments
![]()
Labels: health bits, Neurocystercercosis, Parasites, Taenia Solium
Wednesday, November 19, 2008
The Heart of the Matter
Teen lives 4 months with no heart, leaves hospital
By RASHA MADKOUR, Associated Press Writer
MIAMI – D'Zhana Simmons says she felt like a "fake person" for 118 days when she had no heart beating in her chest. "But I know that I really was here," the 14-year-old said, "and I did live without a heart."
As she was being released Wednesday from a Miami hospital, the shy teen seemed in awe of what she's endured. Since July, she's had two heart transplants and survived with artificial heart pumps — but no heart — for four months between the transplants.
Last spring D'Zhana and her parents learned she had an enlarged heart that was too weak to sufficiently pump blood. They traveled from their home in Clinton, S.C. to Holtz Children's Hospital in Miami for a heart transplant.
But her new heart didn't work properly and could have ruptured so surgeons removed it two days later.
And they did something unusual, especially for a young patient: They replaced the heart with a pair of artificial pumping devices that kept blood flowing through her body until she could have a second transplant.
Dr. Peter Wearden, a cardiothoracic surgeon at Children's Hospital of Pittsburgh who works with the kind of pumps used in this case, said what the Miami medical team managed to do "is a big deal."
"For (more than) 100 days, there was no heart in this girl's body? That is pretty amazing," Wearden said.
The pumps, ventricular assist devices, are typically used with a heart still in place to help the chambers circulate blood. With D'Zhana's heart removed, doctors at Holtz Children's Hospital crafted substitute heart chambers using a fabric and connected these to the two pumps.
Although artificial hearts have been approved for adults, none has been federally approved for use in children. In general, there are fewer options for pediatric patients. That's because it's rarer for them to have these life-threatening conditions, so companies don't invest as much into technology that could help them, said Dr. Marco Ricci, director of pediatric cardiac surgery at the University of Miami.
He said this case demonstrates that doctors now have one more option.
"In the past, this situation could have been lethal," Ricci said.
And it nearly was. During the almost four months between her two transplants, D'Zhana wasn't able to breathe on her own half the time. She also had kidney and liver failure and gastrointestinal bleeding.
Taking a short stroll — when she felt up for it — required the help of four people, at least one of whom would steer the photocopier-sized machine that was the external part of the pumping devices.
When D'Zhana was stable enough for another operation, doctors did the second transplant on Oct. 29.
"I truly believe it's a miracle," said her mother, Twolla Anderson.
D'Zhana said now she's grateful for small things: She'll see her five siblings soon, and she can spend time outdoors.
"I'm glad I can walk without the machine," she said, her turquoise princess top covering most of the scars on her chest. After thanking the surgeons for helping her, D'Zhana began weeping.
Doctors say she'll be able to do most things that teens do, like attending school and going out with friends. She will be on lifelong medication to keep her body from rejecting the donated heart, and there's a 50-50 chance she'll need another transplant before she turns 30.
For now, though, D'Zhana is looking forward to celebrating another milestone. On Saturday, she turns 15 and plans to spend the day riding in a boat off Miami's coast.
Posted by
albularyo
at
10:30 AM
1 comments
![]()
Labels: Medical News, Organ transplant
Wednesday, November 12, 2008
Bone marrow transplant suppresses AIDS in patient
BERLIN (Reuters) - A bone marrow transplant using stem cells from a donor with natural genetic resistance to the AIDS virus has left an HIV patient free of infection for nearly two years, German researchers.
The patient, an American living in Berlin, was infected with the human immunodeficiency virus that causes AIDS and also had leukemia. The best treatment for the leukemia was a bone marrow transplant, which takes the stem cells from a healthy donor's immune system to replace the patient's cancer-ridden cells.
Dr. Gero Hutter and Thomas Schneider of the Clinic for Gastroenterology, Infections and Rheumatology of the Berlin Charite hospital said on Wednesday the team sought a bone marrow donor who had a genetic mutation known to help the body resist AIDS infection.
The mutation affects a receptor, a cellular doorway, called CCR5 that the AIDS virus uses to get into the cells it infects.
When they found a donor with the mutation, they used that bone marrow to treat the patient. Not only did the leukemia disappear, but so did the HIV.
"As of today, more than 20 months after the successful transplant, no HIV can be detected in the patient," the clinic said in a statement.
"We performed all tests, not only with blood but also with other reservoirs," Schneider told a news conference.
"But we cannot exclude the possibility that it's still there."
The researchers stressed that this would never become a standard treatment for HIV. Bone marrow stem cell transplants are rigorous and dangerous and require the patient to first have his or her own bone marrow completely destroyed.
Patients risk death from even the most minor infections because they have no immune system until the stem cells can grow and replace their own.
HIV has no cure and is always fatal. Cocktails of drugs can keep the virus suppressed, sometimes to undetectable levels. But research shows the virus never disappears -- it lurks in so-called reservoirs throughout the body.
Hutter's team said they have been unable to find any trace of the virus in their 42-year-old patient, who remains unnamed, but that does not mean it is not there.
"The virus is tricky. It can always return," Hutter said.
The CCR5 mutation is found in about 3 percent of Europeans, the researchers said. They said the study suggests that gene therapy, a highly experimental technology, might someday be used to help treat patients with HIV.
(Reporting by Oliver Denzer; Writing by Maggie Fox in Washington; Editing by Vicki Allen)
Posted by
albularyo
at
2:01 PM
1 comments
![]()
Labels: AIDS, Bone Marrow Transplant, HIV, Medical News, Stem Cell Research
Tuesday, November 11, 2008
Nursing board exam ‘leakage-free’--execs
By Tetch Torres
INQUIRER.net
First Posted 14:01:00 11/11/2008
MANILA, Philippines -- The nursing board exam this November will be “leakage-free,” according to officials of the Board of Nursing, amid reports that one of the review centers have released some items in the tests scheduled for the 29th and 30th.
Carmencita Abaquin, BON chairperson, and member Marco Sto. Tomas, assured the public that they have taken the necessary steps to ensure the credibility of the forthcoming licensure exam.
They disclosed that text messages being circulated said that a review center has leaked parts of the test in Baguio, Cebu, and Surigao and that members of the Professional Regulatory Commission (PRC) -- one former, the other incumbent -- were behind this.
But Sto. Tomas said security measures have been adopted to prevent a repeat of the June 2006 scandal. These include the quarantine of the members of the PRC and BON from the time the questionnaires are “extracted, printed, and sealed.”
Sto. Tomas said 500 questions per test have been encoded into the computer. These will enter certain parameters/framework per competency (for the 5 tests) and the computer will extract these questions based on the framework by which they have been entered.
"All these are done under quarantine meaning we have no communication outside," Sto. Tomas said.
And then the questions will be extracted, printed, and sealed, he said.
Printing has been centralized unlike during the board exam controversy in 2006 when printing was done per region.
In transporting of questionnaires, there will be escorts from the Philippine National Police (PNP) and National Bureau of Investigation (NBI), Sto. Tomas said.
"These text messages from review centers are only using the leakage as a marketing ploy to entice examinees. They are capitalizing on what happened years ago and the PRC is suffering from this scheme," Abaquin said.
The BON is coordinating with the nursing schools, as well as the Commission on Higher Education (CHED), to implement strict measures to make sure that the country will have high quality nurses, Sto. Tomas said.
There are a total of 88,750 nursing graduates set to take the second licensure examination on November 29 and 30, with the figure considered to be the highest in PRC history.
The BON will go on quarantine starting November 19.
Posted by
albularyo
at
6:31 AM
1 comments
![]()
Labels: NLE, Nursing News
Monday, November 10, 2008
V for Venipuncture
Such a simple procedure really but the most overlooked one. Remember to always follow the Universal precaution otherwise you will be in trouble with The Joint Commission on the Accreditation of Healthcare Organizations (JCAHO). :)
video credits: PocketSnips
Posted by
albularyo
at
7:04 PM
0
comments
![]()
Labels: Bedside Procedures, Venipuncture
Sunday, November 9, 2008
NCLEX Tips
NCLEX Sample Questions
1. A nurse is working in an outpatient orthopedic clinic. During the patient’s history the patient reports, “I tore 3 of my 4 Rotator cuff muscles in the past.” Which of the following muscles cannot be considered as possibly being torn?
A: Teres minor
B: Teres major
C: Supraspinatus
D: Infraspinatus
2. A nurse at outpatient clinic is returning phone calls that have been made to the clinic. Which of the following calls should have the highest priority for medical intervention?
A: A home health patient reports, “I am starting to have breakdown of my heels.”
B: A patient that received an upper extremity cast yesterday reports, “I can’t feel my fingers in my right hand today.”
C: A young female reports, ”I think I sprained my ankle about 2 weeks ago.”
D: A middle-aged patient reports, ”My knee is still hurting from the TKR.”
3. A nurse working a surgical unit, notices a patient is experiencing SOB, calf pain, and warmth over the posterior calf. All of these may indicate which of the following medical conditions?
A: Patient may have a DVT.
B: Patient may be exhibiting signs of dermatitis.
C: Patient may be in the late phases of CHF.
D: Patient may be experiencing anxiety after surgery.
4. A nurse is performing a screening on a patient that has been casted recently on the left lower extremity. Which of the following statements should the nurse be most concerned about?
A: The patient reports, “I didn’t keep my extremity elevated like the doctor asked me to.”
B: The patient reports, “I have been having pain in my left calf.”
C: The patient reports, “My left leg has really been itching.”
D: The patient reports, “The arthritis in my wrists is flaring up, when I put weight on my crutches.”
5. A 93 year-old female with a history of Alzheimer’s Disease gets admitted to an Alzheimer’s unit. The patient has exhibited signs of increased confusion and limited stability with gait. Moreover, the patient is refusing to use a w/c. Which of the following is the most appropriate course of action for the nurse?
A: Recommend the patient remain in her room at all times.
B: Recommend family members bring pictures to the patient’s room.
C: Recommend a speech therapy consult to the doctor.
D: Recommend the patient attempt to walk pushing the w/c for safety.
6. A nurse is covering a pediatric unit and is responsible for a 15 year-old male patient on the floor. The mother of the child states, “I think my son is sexually interested in girls.” The most appropriate course of action of the nurse is to respond by stating:
A: “I will talk to the doctor about it.”
B: “Has this been going on for a while?”
C: “How do you know this?”
D: “Teenagers often exhibit signs of sexual interest in females.”
7. A high school nurse observes a 14 year-old female rubbing her scalp excessively in the gym. The most appropriate course of action for the nurse to do is:
A: Request a private evaluation of the female’s scalp from her parents.
B: Contact the female’s parents about your observations.
C: Observe the hairline and scalp for possible signs of lice.
D: Contact the student’s physician.
8. A nurse is caring for a patient who has recently been diagnosed with fibromyalgia and COPD. Which of the following tasks should the nurse delegate to a nursing assistant?
A: Transferring the patient to the shower.
B: Ambulating the patient for the first time.
C: Taking the patient’s breath sounds
D: Educating the patient on monitoring fatigue
9. A nurse has been instructed to place an IV line in a patient that has active TB & HIV. The nurse should where which of the following safety equipment?
A: Sterile gloves, mask, and goggles
B: Surgical cap, gloves, mask, and proper shoewear
C: Double gloves, gown, and mask
D: Goggles, mask, gloves, and gown
10. A nurse is instructing a person who had a left CVA and right lower extremity hemiparesis to use a quad cane. Which of the following is the most appropriate gait sequence?
A: Place the cane in the patient’s left upper extremity, encourage cane, then right lower extremity, then left upper extremity gait sequence.
B: Place the cane in the patient’s left upper extremity, encourage cane, then left lower extremity, then right upper extremity gait sequence.
C: Place the cane in the patient’s right upper extremity, encourage cane, then right lower extremity, then left upper extremity gait sequence.
D: Place the cane in the patient’s right upper extremity, encourage cane, then left lower extremity, then right upper extremity gait sequence.
11. A nurse has just started on the 7PM surgical unit shift. Which of the following patients should the nurse check on first?
A: A 75 year-old female who is scheduled for an EGD in 10 hours.
B: A 34 year-old male who is complaining of low back pain following back surgery and has an onset of urinary incontinence in the last hour.
C: A 21 year-old male who had a lower extremity BKA yesterday, following a MVA and has phantom pain.
D: A 27 year-old female who has received 1.5 units of RBC’s. via transfusion the previous day.
12. A 64 year-old Alzheimer’s patient has exhibited excessive cognitive decline resulting in harmful behaviors. The physician orders restraints to be placed on the patient. Which of the following is the appropriate procedure?
A: Secure the restraints to the bed rails on all extremities.
B: Notify the physician that restraints have been placed properly.
C: Communicate with the patient and family the need for restraints.
D: Position the head of the bed at a 45 degree angle.
13. A 22 year-old patient in a mental health lock-down unit under suicide watch appears happy about being discharged. Which of the following is probably happening?
A: The patient is excited about being around family again.
B: The patient’s suicide plan has probably progressed.
C: The patient’s plans for the future have been clarified.
D: The patient’s mood is improving.
14. A patient that has delivered a 8.2 lb. baby boy 3 days ago via c-section, reports white patches on her breast that aren’t going away. Which of the following medications may be necessary?
A: Nystatin
B: Atropine
C: Amoxil
D: Loritab
15. A 13 year old girl is admitted to the ER with lower right abdominal discomfort. The admitting nursing should take which the following measures first?
A: Administer Loritab to the patient for pain relief.
B: Place the patient in right sidelying position for pressure relief.
C: Start a Central Line.
D: Provide pain reduction techniques without administering medication.
16. A 64 year-old male who has been diagnosed with COPD, and CHF exhibits an increase in total body weight of 10 lbs. over the last few days. The nurse should:
A: Contact the patient’s physician immediately.
B: Check the intake and output on the patient’s flow sheet.
C: Encourage the patient to ambulate to reduce lower extremity edema.
D: Check the patient’s vitals every 2 hours.
17. A 32 year-old male with a complaint of dizziness has an order for Morphine via IV. The nurse should do which of the following first?
A: Check the patient’s chest x-ray results.
B: Retake vitals including blood pressure.
C: Perform a neurological screen on the patient.
D: Request the physician on-call assess the patient.
18. A patient that has TB can be taken off restrictions after which of the following parameters have been met?
A: Negative culture results.
B: After 30 days of isolation.
C: Normal body temperature for 48 hours.
D: Non-productive cough for 72 hours.
19. A nurse teaching a patient with COPD pulmonary exercises should do which of the following?
A: Teach purse-lip breathing techniques.
B: Encourage repetitive heavy lifting exercises that will increase strength.
C: Limit exercises based on respiratory acidosis.
D: Take breaks every 10-20 minutes with exercises.
20. A patient asks a nurse the following question. Exposure to TB can be identified best with which of the following procedures? Which of the following tests is the most definitive of TB?
A: Chest x-ray
B: Mantoux test
C: Breath sounds examination
D: Sputum culture for gram-negative bacteria
Answer Key
1. (B) Teres Minor, Infraspinatus, Supraspinatus, and Subscapularis make up the Rotator Cuff.
2. (B) The patient experiencing neurovascular changes should have the highest priority. Pain following a TKR is normal, and breakdown over the heels is a gradual process. Moreover, a subacute ankle sprain is almost never a medical emergency.
3. (A) All of these factors indicate a DVT.
4. (B) Pain may be indicating neurovascular complication.
5. (B) Stimulation in the form of pictures may decrease signs of confusion.
6. (D) Adolescents exhibiting signs of sexual development and interest are normal.
7. (C) Observation of the student’s hair is the next step.
8. (A) Nursing assistants should be competent on all transfers.
9. (D) All protective measures must be worn, it is not required to double glove.
10. (A) The cane should be placed in the patient’s strong upper extremity, and left arm/right foot go together, for normal gait.
11. (B) The new onset of urinary incontinence may require additional medical assessment, and the physician needs to be notified.
12. (C) Both the family and the patient should have the need for restraints explained to them.
13. (B) The suicide plan may have been decided.
14. (A) Thrush may be occurring and the patient may need Nystatin.
15. (D) Do not administer pain medication or start a central line without MD orders.
16. (B) Check the intake and output prior to making any decisions about patient care.
17. (B) Dizziness can be a sign of hypotension, that may a contraindication with Morphine.
18. (A) Negative culture results would indicate absence of infection.
19. (A) Purse lip breathing will help decrease the volume of air expelled by increased bronchial airways.
20. (B) The Mantoux is the most accurate test to determine the presence of TB
Source: Test Trade
Posted by
albularyo
at
2:45 AM
0
comments
![]()
Labels: NCLEX Tips
Thursday, October 23, 2008
The Placebo Effect

Survey: Half of US doctors use placebo treatments
By MARIA CHENG, AP Medical Writer
LONDON – About half of American doctors in a new survey say they regularly give patients placebo treatments — usually drugs or vitamins that won't really help their condition. And many of these doctors are not honest with their patients about what they are doing, the survey found.
That contradicts advice from the American Medical Association, which recommends doctors use treatments with the full knowledge of their patients.
"It's a disturbing finding," said Franklin G. Miller, director of the research ethics program at the U.S. National Institutes Health and one of the study authors. "There is an element of deception here which is contrary to the principle of informed consent."
The study was being published online in Friday's issue of BMJ, formerly the British Medical Journal.
Placebos as defined in the survey went beyond the typical sugar pill commonly used in medical studies. A placebo was any treatment that wouldn't necessarily help the patient.
Scientists have long known of the "placebo effect," in which patients given a fake or ineffective treatment often improve anyway, simply because they expected to get better.
"Doctors may be under a lot of pressure to help their patients, but this is not an acceptable shortcut," said Irving Kirsch, a professor of psychology at the University of Hull in Britain who has studied the use of placebos.
Researchers at the NIH sent surveys to a random sample of 1,200 internists and rheumatologists — doctors who treat arthritis and other joint problems. They received 679 responses. Of those doctors, 62 percent believed that using a placebo treatment was ethically acceptable.
Half the doctors reported using placebos several times a month, nearly 70 percent of those described the treatment to their patients as "a potentially beneficial medicine not typically used for your condition." Only 5 percent of doctors explicitly called it a placebo treatment.
Most doctors used actual medicines as a placebo treatment: 41 percent used painkillers, 38 percent used vitamins, 13 percent used antibiotics, 13 percent used sedatives, 3 percent used saline injections, and 2 percent used sugar pills.
In the survey, doctors were asked if they would recommend a sugar pill for patients with chronic pain if it had been shown to be more effective than no treatment. Nearly 60 percent said they would.
Smaller studies done elsewhere, including Britain, Denmark and Sweden, have found similar results.
Jon Tilburt, the lead author of the U.S. study, who is with NIH's bioethics department, said he believes the doctors surveyed were representative of internists and rheumatologists across the U.S. No statistical work was done to establish whether the survey results would apply to other medical specialists, such as pediatricians or surgeons.
The research was paid for by NIH's bioethics department and the National Center for Complementary and Alternative Medicine.
The authors said most doctors probably reasoned that doing something was better than doing nothing.
In some cases, placebos were given to patients with conditions such as chronic fatigue syndrome. Doctors also gave antibiotics to patients with viral bronchitis, knowing full well that a virus is impervious to antibiotics, which fight bacteria. Experts believe overuse of antibiotics promotes the development of drug-resistant strains of bacteria.
Some doctors believe placebos are a good treatment in certain situations, as long as patients are told what they are being given. Dr. Walter Brown, a professor of psychiatry at Brown and Tufts universities, said people with insomnia, depression or high blood pressure often respond well to placebo treatments.
"You could tell those patients that this is something that doesn't have any medicine in it but has been shown to work in people with your condition," he suggested.
However, experts don't know if the placebo effect would be undermined if patients were explicitly told they were getting a dummy pill.
Brown said that while he hasn't prescribed sugar pills, he has given people with anxiety problems pills that had extremely low doses of medication. "The dose was so low that whatever effect the patients were getting was probably a placebo effect," he said.
Kirsch, the psychologist, said it might be possible to get the psychological impact without using a fake pill. "If doctors just spent more time with their patients so they felt more reassured, that might help," he said.
Some patients who had just seen their doctors at a clinic in London said the truth was paramount.
"I would feel very cheated if I was given a placebo," said Ruth Schachter, an 86-year-old Londoner with skin cancer. "I like to have my eyes wide open, even if it's bad news," she said. "If I'm given something without being warned what it is, I certainly would not trust the doctor again."
The Pros vis-à-vis Cons notwithstanding; Let us just remember that the Doctor- Patient relationship is sacred. Honesty is always the best policy in dealing with patients especially with regards to their treatments.
Posted by
albularyo
at
10:04 PM
1 comments
![]()
Labels: Medical Ethics, Medical Issues, Placebo
Tuesday, October 21, 2008
Clinical Eye

Here are some of the latest news that caught my eyes...
General Anesthesia Tied to Developmental Woes in Kids
Youngsters under the age of 3 who had hernia surgery showed almost twice the risk of behavioral or developmental problems later compared to kids who hadn't had surgery, a new study finds.
Researchers suspect that exposure to general anesthesia during these operations might have played a role in the jump in risk, according to lead author Charles DiMaggio, an assistant professor of clinical epidemiology at Columbia University College of Physicians and Surgeons' Mailman School of Public Health in New York City. More...
Dr. Marc Bessler, right, and Dr. Daniel Davis performed a new kind of weight-loss surgery that passes a stapler down the throat to staple the stomach.
Toga (for transoral gastroplasty) is a new weight-loss surgery... click herefor more.
Magnet device aims to treat depression patients...
If it sounds like science-fiction, well, those woodpecker-like pulses trigger small electrical charges that spark brain cells to fire. Yet it doesn't cause the risks of surgically implanted electrodes or the treatment of last resort, shock therapy.
Called transcranial magnetic stimulation or TMS, this gentler approach isn't for everyone. The Food and Drug Administration approved Neuronetics Inc.'s NeuroStar therapy specifically for patients who had no relief from their first antidepressant, offering them a different option than trying pill after pill.
Read the entire article, here.
Posted by
albularyo
at
8:15 PM
0
comments
![]()
Labels: Medical News
Monday, October 13, 2008
Pain in My Heart

VIOXX- pain killer or heart killer?
The painful saga of the pain medicine continues...
Vioxx's Heart Risk Lingered Long After Use Ended
By Steven Reinberg
HealthDay Reporter
MONDAY, Oct. 13 (HealthDay News) -- When the pain killer Vioxx was pulled from the market in 2004 over concerns that it increased the risk of heart attack, stroke and death, many assumed that stopping the drug would end the risk.
But a new study finds that "the risk was increased close to twofold, and the risk persisted for approximately a year," said co-author Dr. Robert Bresalier, a professor of medicine at the M.D. Anderson Cancer Center in Houston.
"The good news is that, after a year, the risk seemed to go back down toward normal," he said.
However, the study's researchers and other experts also believe that long-term use of most non-aspirin painkilling drugs in this class -- called non-steroidal anti-inflammatory drugs (NSAIDs) -- also boost users' risks of heart attack, stroke and death to some degree.
NSAIDs include cox-2 inhibitor drugs such as the now-banned Vioxx and Bextra, as well as the remaining cox-2 on the market, Celebrex. Those drugs target the cyclooxygenase 2 (cox-2) enzyme involved in inflammation.
NSAIDs also include less targeted anti-inflammatory medications such as ibuprofen (Advil, Motrin) and naproxen (Aleve).
The report was published online in the Oct. 14 issue of The Lancet.
For the study, Bresalier's group followed people who had participated in the international APPROVe trial, which compared Vioxx to placebo over 3 years in an attempt to see whether the drug could cut the recurrence of cancerous colon polyps. The trial was stopped early in 2004 because of the increased risk for heart attacks and stroke.
The researchers in the new study were able to contact 84 percent of the almost 2,600 people who had participated in the trial.
They found that a year after discontinuing Vioxx, ex-users still had a 79 percent increased risk of heart attack, stroke or death compared with those who had received placebo.
This finding was consistent with the increased risk observed during the trial, where the odds for cardiovascular trouble was more than double for those taking Vioxx. For individual patients, the risk of heart attack or stroke was doubled during the year after stopping the drug. The increased risk of dying was 31 percent compared with those who had taken placebo, the researchers noted.
Bresalier's group did find that Vioxx was able to reduce the recurrence of colon polyps, but this benefit has to be weighed against the increase in cardiovascular risk, they said.
Bresalier suspects that long-term use of all non-aspirin NSAIDs can raise the odds of cardiovascular trouble to some extent.
"Similar data has been evident for some of the other cox-2 inhibitors," he noted. "In fact, it seems to be a class effect for most if not all NSAIDs. There is a dose-dependent risk with Celebrex as well, whose magnitude was not that much different from Vioxx," he said.
Bresalier believes that certain patients should not take high doses of these drugs over a long period. "If you have a history of cardiovascular disease, speak to your doctor to understand the relative risks and benefits. If you're somebody who really needs to take these drugs because of chronic pain or severe arthritis, be aware of the issues. But you shouldn't be afraid to take these drugs if you need them," he said.
For people who take these drugs only intermittently -- for short-term pain relief, for example -- the risk is very small, Bresalier said. "It doesn't mean if you take one or two pills you're going to get a heart attack. For the vast majority of people taking these drugs, these are very good and safe drugs," he said.
Dr. Eric J. Topol, director of the Scripps Translational Science Institute and Chief Academic Officer of Scripps Health in La Jolla, Calif., was not surprised that the risk for heart attack and stroke continued even after Vioxx was stopped.
"What this does is help further demonstrate not only the risk of Vioxx, but the temporal duration," Topol said. "Now, we have compelling data that the risk extends a year after stopping the drug," he said.
Topol, who was one of the first to sound the alarm about Vioxx, is not sure that this is a class effect of all cox-2 inhibitors, however.
"There was always a signal that it [the risk] was worse for Vioxx that other cox-2 inhibitors. Whether or not other drugs like Celebrex shared that isn't known. That has not been demonstrated in studies of Celebrex. But you have to be suspicious, particularly since high doses of Celebrex have heart attack and stroke risk. But there's never been a study to show that it's a long-lasting liability," he said.
In response to the Lancet study, Vioxx manufacturer Merck issued the following statement: "Merck believes that this post-hoc analysis using limited data from a prematurely terminated study needs to be interpreted very cautiously and in the context of the rest of the data from the extensive clinical development program for Vioxx."
Posted by
albularyo
at
9:18 PM
1 comments
![]()
Labels: Bad Medicine, health bits, Vioxx
Sunday, October 5, 2008
THINGS YOU DON’T WANT TO HEAR IN SURGERY

- Better save that. We'll need it for the autopsy.
- "Accept this sacrifice, O Great Lord of Darkness!"
- Wait a minute, if this is his spleen, then what's that?
- Hand me that ... uh ... that uh..... thingie
- Oops! Hey, has anyone ever survived 500ml of this stuff before?
- There go the lights again...
- "Ya know, there's big money in kidneys… and this guy's got two of'em.
- Everybody stand back! I lost my contact lens!
- Could you stop that thing from beating? It's throwing my concentration off.
- What's this doing here?
- I hate it when they're missing stuff in here.
- That's cool! Now can you make his leg twitch?!
- Well folks, this will be an experiment for all of us.
- Sterile, shcmerile. The floor's clean, right?
- The “5-second rule” applies to organs, too – right?
- What do you mean he wasn't in for a sex change...
- “Oh, you mean HIS right…”
- OK, now take a picture from this angle. This is truly a freak of nature.
- This patient has already had some kids, am I correct?
- Nurse, did this patient sign the organ donation card?
- Don't worry. I think it is sharp enough.
- What do you mean "You want a divorce"!?!
- FIRE! FIRE! Everyone get out!
- Damn! Page 47 of the manual is missing!
Posted by
albularyo
at
2:03 AM
0
comments
![]()
Labels: Humor in Medicine
Wednesday, October 1, 2008
Warts Up, Doc?

Doctors were at a loss for explanations when an Indonesian fisherman grew warts out of his arms and feet that resembled tree branches. But according to Britain's The Sun newspaper, Dede's growths are going away, thanks to the help of an American dermatologist.
--SUPRI, Reuters / Corbis
Posted by
albularyo
at
11:11 PM
0
comments
![]()
Labels: Rare Medical Disorder
Monday, September 29, 2008
NCLEX Tips
NCLEX is quite easy if you know what to study and you prepare really well for it. NCLEX is designed to pass the student rather than to fail them.
Its purpose is to test your understanding of what you already learned, it all boils down on what you know, and that’s why preparation is the sole most important factor of passing the test.
That’s why my advice is for you to read and read and read…
Unfortunately, memorization doesn’t work out that well in this case since if you’re going to memorize everything you will end up as one dazed and confused examinee.
Rather it is the way you prepare and approach the issue. Instead of memorizing those kilometric explanations and descriptions in the book, it will do you more good to take notes of what you deem are important in every topic/ system that you encounter in your review. Familiarization and repetition of critical concepts in Nursing will surely help you pass the exam.
Thus, making some flash cards will be of much help in this particular case.
Here are some topics that I found on the net which will help you in passing the NCLEX. Learn about them and they will make your life come examination day really easy.
* Types of Nosocomial Infections
* Principles of Surgical Asepsis
* Medical Testing and Labs
* TURP Procedure
* Romberg’s Test
* Lithotripsy Procedure
* Levels of Consciousness
* Mental Exam Basics
* Grading of Deep Tendon Reflexes
* Glascow Coma Scale
* Normative Values
* Methods of Oxygen Delivery
* Dementia and Delirium
* Types of Injections
* Ethical Duties of Nurses
* Patient Rights
* Bioethical Principles
* Changes Associated with Aging
* Drip Rate Calculations
* Barriers to Communication
* Nutrition and TPN
* Attributes of Nutrients
* Methods of Absorption
* Metabolism and Nutrition
* Medical Nutrition Therapy
* Cultural Aspects of Diets
* Placenta Previa
* Stages of Labor
* Assessing Fetal Lung Maturity
* Pathology of Eclampsia
* PMS and Menopause
* Attributes of Battered Women
* Apgar Scores
* Types of Cardiomyopathies
* Opportunistic Infections
* Classifications of Cancer
* Medical Nutritional Therapy
* Staging of Pressure Ulcers
* Disease Pathology
* Types of Shock
* Lipid Profile Labs
* Coagulation Studies
* CBC Components
* Acne Treatment Medications
* Phases of Adolescence
* Three Types of Jaundice
* Pain Assessment
* Lymphoma Characteristics
* Sexually Transmitted Diseases
* Tanner Staging
* Vaccinations and Immunizations
* Symptoms of Child Abuse
* Performing Newborn Assessments
* Motor Development
* Development of Language
* Pharmacology
* Types of Adrenergic Receptors
* Properties of Decongestants
* Classifications of Drugs
* Antipsychotic Classifications
* Drug Interactions
* Major Injection Sites
* Calcium Channel Blockers
* Phases of Burn Management
* Types of Burns
* Wound Healing Phases
Here's an example of what a flash card should look like (Click on the photo for a closer look)--

Posted by
albularyo
at
4:53 PM
2
comments
![]()
Labels: NCLEX Tips
Wednesday, September 24, 2008
To TPA or not to TPA?
That is the question.
Tissue Plasminogen Activator or more commonly TPA is a genetically- engineered blood clot dissolver that was first used to prevent heart damage after a heart attack since the late 1980s and through the years have been one of the mainstays in the treatment of Stroke because of its ability to reduce the long- term disability that usually result from the disease.
TPA is usually given within three hours of a Stroke which is usually known in legal parlance as the “window- period” or “golden hour” to be effective and beyond that there‘s the clear and present danger of bleeding in the brain which is the TPA’s worst complication .
However recent findings by researchers and scientists in the medical field are now reconsidering that old belief and are now concluding that it is still safe to give TPA beyond the so- called “three- hour” window period.
Here's the news from the Associated Press- Study: Extending time of stroke drug treatment OK
And here's the article of the study from the New England Journal of Medicine - Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke
Posted by
albularyo
at
3:48 PM
0
comments
![]()
Labels: health bits, NEJM, Stroke, TPA
Saturday, September 13, 2008
Easy ECG
Even in the advent of modern diagnostic machines in the world of medicine, ECG or EKG remains the fastest and simplest way to look into the heart. It is still very useful especially in the Clinical or Emergency Room settings where a quick determination of the heart’s function is paramount especially in cases of Acute Myocardial Infarction or Heart Attack.
The Electrocardiogram can determine a heart block, enlarged heart muscles and rhythm disturbances. It also helps determine previous cases of heart attack. Thus, the ECG is a valuable tool because it helps diagnose irregularities and changes in the heart as well as to establish a baseline for subsequent ECGs.
Here are some videos that will help you further understand the concept and importance of the Electrocardiogram--
video credits:
Dr. Dean Keller and Dr. Melissa Stiles
University of Wisconsin School of Medicine and Public Health
Posted by
albularyo
at
2:57 PM
0
comments
![]()
Labels: ECG, EKG, Electorcardiogram
Friday, September 12, 2008
Assessing Lung Sounds
Normal Breath Sounds
The correct sequence of auscultation of the posterior chest is shown in the picture below. The sequence is from the apex to the base of the lungs from one side to the other including the lateral areas of the lungs.
Credits: Dr. Pat O'Leary
David W. Woodruff, MSN, RN- BC, CNS, CEN
Posted by
albularyo
at
6:07 PM
1 comments
![]()
Labels: Lung Sounds
Saturday, September 6, 2008
Gastric bypass anatomy leads to diabetes control
The Reuters article below which is about the relationship between gastric bypass and diabetes control further reinforce the phenomenon that many physicians are now encountering in their practice.
I have seen a lot of people who has diabetes and high levels of blood glucose but are now symptom- free after undergoing a gastric bypass. Now, this article will further explain the mechanism behind this new phenomenon.
So, read on…
NEW YORK (Reuters Health) - The rapid and substantial control of diabetes seen after gastric bypass surgery is due, at least in part, to the intestinal rearrangement involved in the procedure, the results of an animal study suggest.
Besides removing a substantial portion of the stomach, gastric bypass also attaches the output of the stomach to the lower intestines. The lower portion of the gut usually produces little glucose, but because of the direct input from the stomach it increases its production, French researchers report in the research journal Cell Metabolism.
The liver senses the higher level of glucose and reduces its own production of the sugar. Since the liver contributes much more to the body's overall glucose production than do the intestines, the net effect is enhanced glucose control, say Dr. Gilles Mithieux, from Universite de Lyon, and colleagues.
The increase in intestinal glucose formation was only noted with gastric bypass, not with gastric banding, which doesn't re-route the intestines. This may explain why only gastric bypass has been associated with enhanced diabetes control, the investigators conclude.
Furthermore, they note, sensors in the liver detect the elevated glucose and send an appetite-suppressing signal to the brain, which contributes to the satiety and weight loss seen with gastric bypass.
SOURCE: Cell Metabolism, September 3, 2008.
Posted by
albularyo
at
4:41 PM
1 comments
![]()
Labels: Diabetes Mellitus, Gastric Bypass
Monday, September 1, 2008
Urethral Catheterization
Urethral catheterization is a frequently performed bed side procedure; if done haphazardly it may lead to infection, particularly if the catheter is left for long periods.
Urethral catheterization is done usually with a balloon tip Foley Catheter of varying sizes (8 Fr* to 26 Fr). The balloon size for most of the applications is designed to hold little over 5 ccs of fluid. Larger Foley catheters with balloon capacity in excess of 30 ccs are available for specific urology purposes. For an average adult sizes 14 to 18 Fr catheters are usually utilized.
Indications for urethral catheterization:
1. Urinary retention (palpable, prominent urinary bladder)
2. To keep the patient dry and manageable when he is obtended or comatose
3. Management of incontinence of urine
4. To watch hourly urine output in intensive care situation.
5. As a part of urologic studies and also managing post operative status.
6. To obtain a catheterized specimen of urine for culture and sensitivity when specially required. (Spontaneously voided midstream specimen is good enough under majority of circumstances and it is rarely necessary to catheterize for diagnosis of UTI).
NOTE: Where there is obvious injury to urethra following trauma Foley catheterization should not be attempted before cystourethrogram is performed.
Procedure:
Although the procedure may vary minimally between male and female patients, the basic principles of aseptic precautions and positioning are essentially the same.
Preliminary hand wash and wearing of cap and mask recommended.
Patient should be in the supine position with legs slightly apart for the male and with legs apart and knees flexed for the female patient.
A preliminary soap and water wash to the external genitalia is desirable.
From this point all procedures are done with sterile gloves.
External preparation of genitalia is performed using betadine pain and sterile drapes are laid to provide adequate exposure to the external genitalia.
Appropriate catheter is picked up and the integrity of the balloon is checked by introducing 5 cc of water into the balloon and deflated.
The sterile catheter is lubricated adequately with sterile jelly lubricant.
Catheterization of the male patient:
The penis is held with the left hand away from the scrotum and holding the catheter firmly with the right hand the well lubricated catheter is gently passed through the external urethral meatus. This is gently and gradually advanced and under most circumstances it is passed through the urinary sphincter without any problem.
Occasionally some resistance may be encountered at the level of the sphincter due to prostatic hypertrophy. By gently advancing further through the sphincter this can be overcome to some extent and catheter can be passed into the bladder.
Occasionally a larger catheter or a “coude” type of catheter may be required to overcome this obstruction. When the catheter passes into the bladder, urine will be seen coming through the catheter. At this point, it is advanced by another 1 to 2 cms and the balloon is inflated with 5 cc or sterile water.
The Foley catheter after collecting specimens for urinalysis and culture is then connected to the Foley bag. Some physicians prefer to apply betadine ointment at the external urethral orifice. The Foley catheter may be stabilized to the medial aspect of one of the thighs using adhesive tapes. This prevents the Foley catheter advancing more towards the bladder thereby carrying infection and also prevents it from unnecessary movements causing discomforts.
Catheterization of the female patient:
In the female, the vulval outlet and labia are carefully washed and painted with betadine and appropriate sterile drapes are laid. With the left hand exposing the urethral meatus by separating the labia with the thumb and index fingers the external urethral meatus is identified and previously lubricated catheter is carefully and gently advanced through it into the bladder.
Care should be taken not to contaminate the catheter by touching the unprepared parts of the genitalia and the vagina. Once the catheter is well placed inside the bladder and the urine is seen coming out of the tube the balloon is distended with 5 cc of sterile water and catheter connected and fixed as described earlier.
Post Catheterization management has to be carefully planned to avoid infections. Except in selected patients, routine antibiotic administration is not necessary. Catheter care and change of catheters when necessary should be remembered. In a hospital set up, catheter induced nosocomial infections of the urinary tract are fairly common. When prolonged catheterization is required appropriate urological and where necessary neurological consultations are obtained to plan long term management of the catheter dependent patient. Ambulatory patients who have Foley catheters left in situ are given appropriate instructions and training in the care of the catheters and also plan periodical visits to the doctors and health care staff.
Note: Consider – use of silicon coated catheter for long-term placements
Credits: NurseReview.Org/ Medindia.net
Posted by
albularyo
at
5:21 PM
0
comments
![]()
Labels: Bedside Procedures
Saturday, August 23, 2008
Face Value
Face transplant patient can smile, blink again 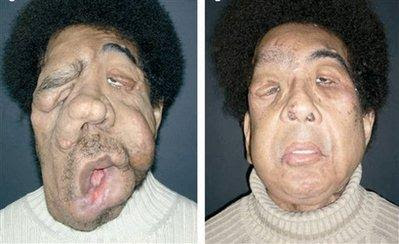
By MARIA CHENG, AP Medical Writer
Fri Aug 22, 7:37 AM ET
LONDON - Transplanting faces may seem like science fiction, but doctors say the experimental surgeries could one day become routine. Two of the world's three teams that have done partial face transplants reported Friday that their techniques were surprisingly effective, though complications exist and more work is still needed.
"There is no reason to think these face transplants would not be as common as kidney or liver transplants one day," said Dr. Laurent Lantieri, one of the French doctors who operated on a man severely disfigured by a genetic disease.
In Friday's issue of the British medical journal Lancet, Lantieri and colleagues reported on their patient's status one year after the transplant. Chinese doctors also reported on their patient, two years after his surgery.
Last year, the French team operated on a 29-year-old man with tumors that blurred his features in a face that looked almost monstrous. They transplanted a new lower face from a donor, giving the patient new cheeks, a nose and mouth. Six months later, he could smile and blink.
The Chinese patient had part of his face ripped off by a bear. Surgeons in Xian gave him a new nose, upper lip and cheek from a donor. After a few months, he could eat, drink and talk normally, and returned home to Yunnan province in southwest China.
The patients were not identified although photos were included in the reports.
As is the case with all transplants, doctors use immune-suppressing drugs to prevent the recipient's body from attacking the donated tissue. In both face transplants, the patients started rejecting the transplanted tissue more than once. Their doctors solved the problem by juggling their medications.
The French patient now takes three pills a day to prevent rejection.
"That's less than most people with diabetes," said Lantieri, a plastic surgeon at the Henri Mondor-Albert Chenevier Hospital in suburban Paris.
Other doctors were reassured by the results.
"To be able to wean down the dosage of the medication in small amounts and relatively quickly, that is encouraging," said Dr. Bohdan Pomahac, a plastic surgeon at the Brigham and Women's Hospital in Boston.
Pomahac has permission to do a face transplant in the U.S., as do doctors at the Cleveland Clinic.
Experts have worried that if patients take lifelong anti-rejection drugs after a transplant, their cancer risk will jump. Some also predicted that rejection would destroy the face within a few years. Those fears seem to have been allayed, Pomahac said.
With three successful partial face transplants so far — including the world's first on a woman whose face was bitten off by a dog in France — doctors say that some of the surgery's initial uncertainties, like how functional the new face would be, are being answered.
For example, Lantieri's patient's face was paralyzed by tumors for more than a decade. The French team wasn't sure if nerves could grow after the transplant. But they discovered later their patient could blink, proving the brain was able to restore long-forgotten facial nerve connections.
Not everyone is convinced that face transplants are so revolutionary.
Dr. Patrick Warnke, a plastic surgeon at the University of Kiel in Germany, calls them a "dead-end road," because he doesn't think the rejection problem can be solved. Instead, he hopes to re-grow tissue from patients' own stem cells.
Still, the biggest obstacle to more face transplants may not be scientific, but social.
"When kidney transplants first began, people were reluctant to donate because there were a lot of cultural, social and religious issues," Pomahac said. "This is exactly the same scenario now."
Doctors plan to do more face transplants, but are having a hard time finding donors.
"Everyone says they would accept a face transplant if they were disfigured," Lantieri said. "The real question is, would you be a donor, or would you allow your family member to donate their face? That is the answer we need to change."
___
On the Net:
http://www.lancet.com
Posted by
albularyo
at
1:46 PM
1 comments
![]()
Labels: Lancet, Medical News, Organ transplant
Thursday, August 21, 2008
Philippine Physician Examination Results
TOP TEN PHYSICIANS Board Examinees
1. Marlon Diaz Garcia, Far Eastern University-Nicanor Reyes Medical Foundation -- 88.75%
2. Dave Anthony Pasetes Diomampo, Saint Louis University -- 88.17%
3. Gentry George Teng King, University of Santo Tomas -- 87.42%
Janice Jill Keng Lao, University of the Philippines-Manila -- 87.42%
4. Nemencio Jr Reyes Ronquillo, University of the Philippines-Manila -- 87.17%
Paolo Potato Villanueva, University of Santo Tomas -- 87.17%
5. Allan Louie Espino Cruz, University of Santo Tomas -- 86.92%
6. Philip Blanco Antiporta, University of Santo Tomas -- 86.58%
7. Ma Cristina Dela Cruz Briones, University of Santo Tomas -- 86.42%
8. Lemuel Benedict Robleza Non, University of the Philippines- Manila -- 86.17%
Sheila Jane Tan Zanoria, Cebu Institute of Medicine -- 86.17%
9. Angela Sacayan Apostol, University of the East Ramon Magsaysay Mem. Medical Ctr.-- 86.08%
Karel Ann Alipasa Espejo, University of the Philippines- Manila -- 86.08%
10. Grace Ann Mariano Nicolas, University of Santo Tomas -- 86.00%
Lists of New Physicians--
Dr. A
Dr. B
Dr. C
Dr. D
Dr. E
Dr. F
Dr. G
Dr. H
Dr. I
Dr. J
Dr. K
Dr. L
Dr. M
Dr. N
Dr. O
Dr. P
Dr. Q
Dr. R
Dr. S
Dr. T
Dr. U
Dr. V
Dr. W
Dr. Y
Dr. Z
Posted by
albularyo
at
11:51 AM
1 comments
![]()
Labels: Board of Medicine, Medicine, Physician Licensure Examination
Tuesday, August 19, 2008
The Nurse Notes: Old & New

A new nurse throws up when the patient does. An experienced nurse calls housekeeping when the patient throws up.
A new nurse wears so many pins on their name badge you can't read it. An experienced doesn't wear a name badge for liability reasons.
A new nurse charts too much. An experienced nurse doesn't chart enough.
A new nurse loves to run codes. An experienced nurse makes graduate nurses run to codes.
A new nurse wants everyone to know they are a nurse. An experienced nurse doesn't want anyone to know they are a nurse.
A new nurse keeps details and notes on a notepad. An experienced nurse writes on the back of their hands, paper scraps, napkins, etc.
A new nurse will spend all day trying to re-orient a paient. An experienced nurse will chart the patient is dis-orientated and restrain them.
A new nurse can hear any alarm at 50 yards. An experienced nurse can't hear any alarms at any distance.
A new nurse loves to hear abnormal heart and breath sounds. An experienced nurse doesn't even want to hear about them unless the pt is symptomatic.
A new nurse spends 2 hours giving a patient a bath. An experienced nurse lets the nurse's aide give the patient a bath.
A new nurse thinks people respect nurses. An experienced nurse knows everybody blames everything on the nurse.
A new nurse looks for blood on a bandage hoping they will get to change it. An experienced nurse knows a little blood never hurt anybody.
A new nurse looks for a chance "to work with the family". An experienced nurse AVOIDS the family.
A new nurse expects medications and supplies to be delivered on time. An experienced nurse expects them to be never delivered at all.
A new nurse will spend days bladder training an incontinent patient. An experienced nurse will insert a Foley catheter.
A new nurse always answer their phone. An experienced nurse checks their caller ID before answering their phone.
A new nurse thinks psychiatric patients are interesting. An experienced nurse thinks psychiatric patients are crazy.
A new nurse carries reference books in their bag. An experienced nurse carries magazines, lunch and something else in their bag.
A new nurse doesn't find this funny. An experienced nurse does.......
So, what are you?
Posted by
albularyo
at
2:00 AM
0
comments
![]()
Labels: Humor in Medicine, Nurse Notes
Thursday, August 14, 2008
On Organ Transplants and Medical Ethics
The issue of when to declare a person dead in order to harvest his/ her vital organs so that another person may live is a very delicate one no matter from which angle you look at it. An issue that's hard to ignore and poses a lot of questions and quite a dilemma to all the parties involved.
There’s an on- going debate as to when to declare potential organ donors dead. The old criterion of brain death as the sole determining factor is now being challenged by a lot of people in the medical field. Many of them are now advocating on a new protocol called Cardiocirculatory death as the new basis to declare a person dead.
The New England Journal of Medicine tackle this issue in its August edition and the Associated Press pick up the story. I copied the said article as the link to the NEJM website and posted them here.
So, read on…
Doctors debate when to declare organ donors dead
By STEPHANIE NANO, Associated Press Writer Thu Aug 14, 3:56 PM ET
NEW YORK - A report on three heart transplants involving babies is focusing attention on a touchy issue in the organ donation field: When and how can someone be declared dead?
For decades, organs have typically been removed only after doctors determine that a donor's brain has completely stopped working. In the case of the infants, all three were on life support and showed little brain function, but they didn't meet the criteria for brain death.
With their families' consent, the newborns were taken off ventilators and surgeons in Denver removed their hearts minutes after they stopped beating. The hearts were successfully transplanted, and the babies who got the hearts survived.
"It seemed like there was an unmet need in two situations," said Dr. Mark Boucek, who led the study at Children's Hospital in Denver. "Recipients were dying while awaiting donor organs. And we had children dying whose family wanted to donate, and we weren't able to do it."
The procedure — called donation after cardiac death — is being encouraged by the federal government, organ banks and others as a way to make more organs available and give more families the option to donate.
But the approach raises legal and ethical issues because it involves children and because, according to critics, it violates laws governing when organs may be removed.
As the method has gained acceptance, the number of cardiac-death donations has steadily increased. Last year, there were 793 cardiac-death donors, about 10 percent of all deceased donors, according to United Network for Organ Sharing. Most of those were adults donating kidneys or livers.
"It is a much more common scenario today that it would have been even five years ago," said Joel Newman, a spokesman for the network.
The heart is rarely removed after cardiac death because of worries it could be damaged from lack of oxygen. In brain-death donations, the donor is kept on a ventilator to keep oxygen-rich blood flowing to the organs until they are removed.
The Denver cases are detailed in Thursday's New England Journal of Medicine. The editors, noting the report is likely to be controversial, said they published it to promote discussion of cardiac-death donation, especially for infant heart transplants.
They also included three commentaries and assembled a panel discussion with doctors and ethicists. Many of the remarks related to the widely accepted "dead donor rule" and the waiting time between when the heart stops and when it is removed to make sure that it doesn't start again on its own.
In two of the Denver cases, doctors waited only 75 seconds; the Institute of Medicine has suggested five minutes, and other surgeons use two minutes.
State laws stipulate that donors must be declared dead before donation, based on either total loss of brain function or heart function that is irreversible. Some commentators contended that the Denver cases didn't meet the rule since it was possible to restart the transplanted hearts in the recipients.
"In my opinion, it's an open-and-shut case. They don't have irreversibility, and they don't have death," said Robert Veatch, a professor of medical ethics at Georgetown University.
But others argue the definition of death is flawed, and that more emphasis should be on informed consent and the chances of survival in cases of severe brain damage.
The Denver transplants were done over three years; one in 2004 and two last year. The three donor infants had all suffered brain damage from lack of oxygen when they were born. On average, they were about four days old when life support was ended.
In the first case, doctors waited for three minutes after the heart stopped before death was declared. Then the waiting time was reduced to 75 seconds on the recommendation of the ethics committee to reduce the chances of damage to the heart.
The authors said 75 seconds was chosen because there had been no known cases of hearts restarting after 60 seconds.
The hearts were given to three babies born with heart defects or heart disease. All three survived, and their outcomes were compared to 17 heart transplants done at the hospital during the same time but from pediatric donors declared brain dead.
"We couldn't tell the difference," said Boucek, who's now at Joe DiMaggio Children's Hospital in Hollywood, Fla.
There were nine other potential cardiac-death donors at the hospital during the same period, but there wasn't a suitable recipient in the area for their hearts, the report said.
The parents of one of the infants in the study, David Grooms and Jill Airington-Grooms, faced the devastating news on New Year's Day 2007 that their first child, Addison, had been born with little brain function and wouldn't survive.
After they decided to remove life support, they were asked about organ donation, and quickly agreed.
"The reality was Addison was not going to live," said Jill Airington-Grooms. "As difficult as that was to hear, this opportunity provided us with a ray of hope."
Three days later, Addison was taken off a ventilator and died. Her heart was given to another Denver-area baby, 2-month-old Zachary Apmann, who was born five weeks premature with an underdeveloped heart.
His parents, Rob and Mary Ann Apmann, said they were given several options and decided to wait for a transplant. They agreed they would accept a cardiac-death donation to increase Zachary's chances.
Mary Ann Apmann said she wasn't worried that the first available heart came from a cardiac-death donor.
"At that point, Zachary was so sick. We did have him at home. But we knew it wasn't much longer," she said.
After the transplant on Jan. 4, his condition quickly improved, and his blue lips disappeared.
Now, at 21 months: "He's just a crazy little kid who loves to play and swim and throw rocks," his mother said.
The two families haven't met yet but have been in touch through letters and calls. Coincidentally, David Grooms said he had an older brother who died three days after he was born in the 1970s with the same heart condition as Zachary's. The Grooms now have an 8-month-old daughter, Harper.
"Addison did only live three days in this world, but because of this, she lives on," her mother said.
Here's the link to--
The New England Journal of Medicine
Posted by
albularyo
at
6:30 PM
1 comments
![]()
Labels: Medical Ethics, Medical Issues, Organ transplant
Thursday, July 24, 2008
2008 Philippine Nursing Board Examination Results
COMPLETE LIST OF NURSING LICENSURE EXAM PASSERS
A total of 27,765 out of 64,459 passed the Nurse Licensure Examination held last June 2008. The examination was administered in 10 areas nationwide.
Click on the links below--
List of new Registered Nurses: A
List of new Registered Nurses: B
List of new Registered Nurses: C
List of new Registered Nurses: D
List of new Registered Nurses: E
List of new Registered Nurses: F
List of new Registered Nurses: G
List of new Registered Nurses: H
List of new Registered Nurses: I
List of new Registered Nurses: J
List of new Registered Nurses: K
List of new Registered Nurses: L
List of new Registered Nurses: M
List of new Registered Nurses: N
List of new Registered Nurses: O
List of new Registered Nurses: P
List of new Registered Nurses: Q
List of new Registered Nurses: R
List of new Registered Nurses: S
List of new Registered Nurses: T
List of new Registered Nurses: U
List of new Registered Nurses: V
List of new Registered Nurses: W
List of new Registered Nurses: X
List of new Registered Nurses: Y
List of new Registered Nurses: Z
Posted by
albularyo
at
2:57 PM
0
comments
![]()
Labels: 2008 nursing boards, NLE
Wednesday, July 23, 2008
When Are You Most Likely to Have a Heart Attack?

Heart disease, including heart attack, is the world's No. 1 killer. A person's risk of heart attack depends mostly on a familiar repertoire of factors: exercise, smoking, diet, weight, genes. But our bodies' circadian rhythms also play a role, leaving us more prone to injury during certain hours than others. If you're guessing that the danger zone comes at the end of a stressful workday, guess again. Here to explain is Roberto Manfredini, professor of internal medicine at the University of Ferrara in Italy.
Q: What time of day am I most likely to have a heart attack?
A: The most dangerous times for heart attack and for all kinds of cardiovascular emergency - including sudden cardiac death, rupture or aneurysm of the aorta, pulmonary embolism and stroke - are the morning and during the last phase of sleep. A group from Harvard estimated this risk and evaluated that on average, the extra risk of having a myocardial infarction, or heart attack, between 6 a.m. and noon is about 40%. But if you calculate only the first three hours after waking, this relative risk is threefold.
The cardiovascular system follows a daily pattern that is oscillatory in nature: most cardiovascular functions exhibit circadian changes (circadian is from the Latin circa and diem, meaning "about one day"). Now, a heart attack depends on the imbalance between increased myocardial oxygen demand (i.e., a greater need for oxygen in your heart) and decreased myocardial oxygen supply - or both. And unfortunately, some functions in the first hours of the day require more myocardial oxygen support: waking and commencing physical activities, the peak of the adrenal hormone cortisol [which boosts blood-pressure and blood-sugar levels] and a further increase in blood pressure and heart rate due to catecholamines (adrenaline and noradrenaline), which show a peak when you wake up. All those factors lead to an increase of oxygen consumption but at the same time contribute to the constriction of vessels. So you have reduced vessel size and reduced blood flow to the coronary vessels.
You have to remember that blood coagulation is important in the genesis of what we call thrombi, the blood clots that can block the blood vessels and cut off supply to the heart. When we wake up, platelets, the particles in the blood that make thrombi, are particularly adhesive to the vessels. Usually we have an endogenous system - it's called fibrinolysis - to dissolve the thrombi. But in the morning, the activity of our fibrinolytic system is reduced. So we have a greater tendency to make thrombi that can occlude the coronary vessels. This contributes to further reduction of coronary blood flow. Thus, at the same time that you need more blood flow, you have less.
All these changes, however, probably are not so harmful in healthy people. But for a person with a plaque in the coronary vessel, if these changes occur at the same time and peak at the same time, the final result is a higher risk of heart attack during that specific window of morning hours.
Why is the risk also higher during the last part of sleep? Usually, during the night, the cardiovascular system is "sleeping," which is characterized by low blood pressure and heart rate. But the last stage of sleep - REM, or rapid eye movement, sleep [when we believe most dreaming occurs] - is a risk period for cardiovascular emergencies because when you dream, you have a dramatic increase of activity of the autonomic nervous system - even more than when you are awake. Probably each of us can remember waking up in the morning sometimes feeling very tired. That's because during that stage of dreams, we were running or facing some danger. Your heart was running, so it was consuming oxygen. And for similar reasons to those when you're awake, that activity is risky if you don't have a good vessel system.
It's probably difficult for people to minimize the effects of their own biological rhythms. For example, you cannot avoid your morning risk by simply waking up later. Some researchers have tried an experimental model, in which people were instructed to stay in bed for four hours after they woke up before rising. But the same pattern simply occurred four hours after waking, because the risk is linked to our activities. We can't be afraid of the catecholamines and the peak in blood pressure in the morning. It's part of our physiology. And for healthy people, it's not a problem.
It's important for doctors, however, to remember this risk when we give therapy. Usually people take hypertensive drugs in the morning, when they wake up. But this is already the higher-risk period - so is the last hour of activity of the pill they have taken the day before [and not all pills give 24-hour coverage]. We have to be sure that the pill we're prescribing is still active when patients need it most. It's not as easy as simply asking patients to take pills before bed instead of first thing in the morning, because during sleep we have a low heart rate and blood pressure. If you lower your blood pressure too much during the night, you risk reducing blood supply to the brain, and that can be harmful too
--Laura Blue
TIME.com
Posted by
albularyo
at
3:03 PM
0
comments
![]()
Labels: heart attack








